Listen to a podcast-style summary of this blog post
When we developed PK1Cloud Filings (formerly StateFilings.com), our goal was to solve a problem that many insurance carriers face but often accept as a necessary inefficiency: redundant data entry across filing systems. For years, state filings teams have managed information across SERFF, internal databases, and various tracking tools, often duplicating work and increasing the risk of human error. The case of one top-20 national insurance carrier demonstrates how a centralized solution can transform that status quo – cutting administrative hours in half, reducing filing errors, and increasing operational confidence.
The Compliance Challenge: Duplicative Entry and Manual Workarounds
Before implementing PK1Cloud Filings, this national carrier’s regulatory filings team was performing dual data entry for every submission – once into SERFF and again into an internal Microsoft Access database. While this setup technically fulfilled their needs, it created persistent inefficiencies:
- Over 50 hours each month were spent on duplicative data entry
- Data mismatches were common, introducing unnecessary compliance risks
- Staff time was consumed by low-value administrative work, driving up labor costs
This isn’t a unique situation. Across the industry, insurers often rely on spreadsheets, Access databases, or custom-built systems that are disconnected from SERFF. This fragmentation not only slows down filing teams but also creates barriers to collaboration, version control, and audit transparency.
The PK1Cloud Filings Solution: One Entry, Complete Integration
This carrier transitioned to PK1Cloud Filings as a centralized system of record for all state filings activity. Rather than entering the same data twice, the filing team now inputs it once into PK1Cloud Filings, where it is automatically formatted and transmitted to SERFF. Key platform features contributed to the transformation:
- Bi-directional SERFF integration that pushes and pulls content in real time
- Automated task management and role-based workflows that reduce delays and oversight risks
- Configurable form libraries and templates that streamline new product and rate filings
- Dashboards and notifications that replace manual tracking and disconnected communication
The results speak clearly.
Measurable Gains: Speed, Accuracy, and Cost Reduction
After adopting PK1Cloud Filings, the insurer reported a:
- 52% reduction in data entry time – dropping from over 100 hours to fewer than 50 hours per month
- $45,000+ in annual labor cost savings – based on average hourly wages for compliance professionals
- 70% drop in filing errors – as a result of reduced data duplication and improved consistency
- 3x faster turnaround – helping the carrier respond more quickly to regulatory timelines
- 100% audit readiness – with complete document versioning and visibility into filing activity
These are not abstract benefits. They represent operational improvements that directly impact bottom-line efficiency and regulatory performance.
Industry Context: Why This Matters Now
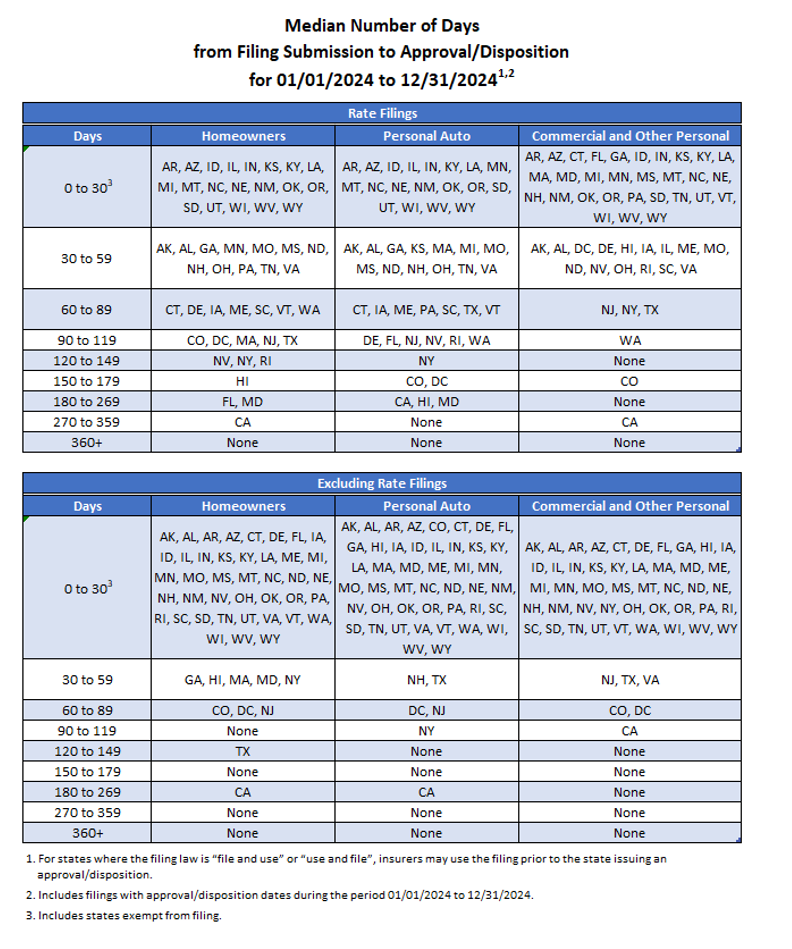
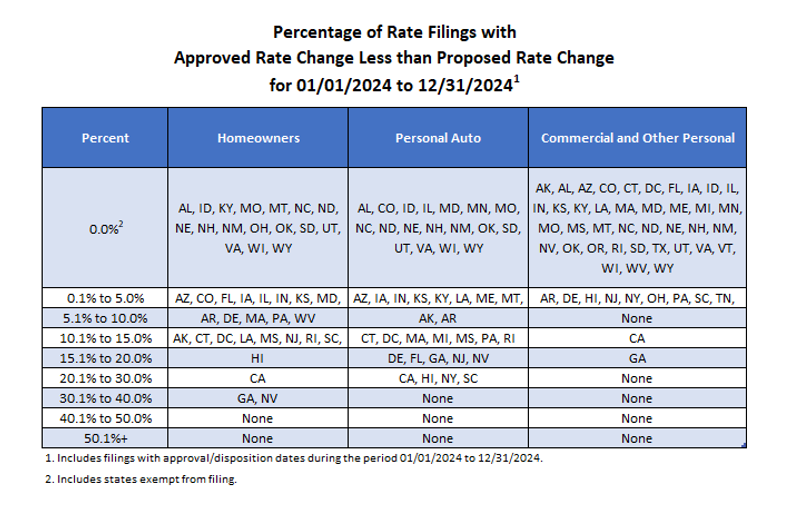
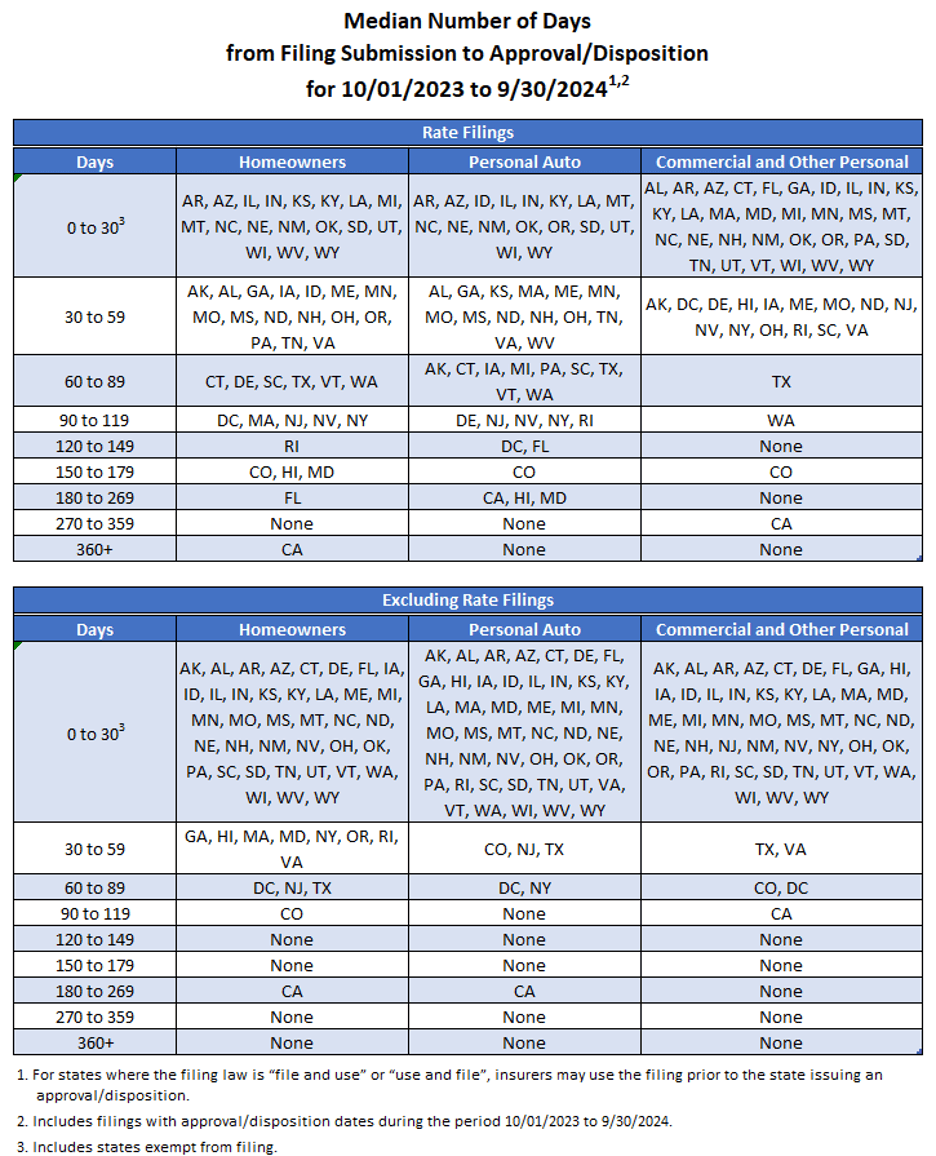
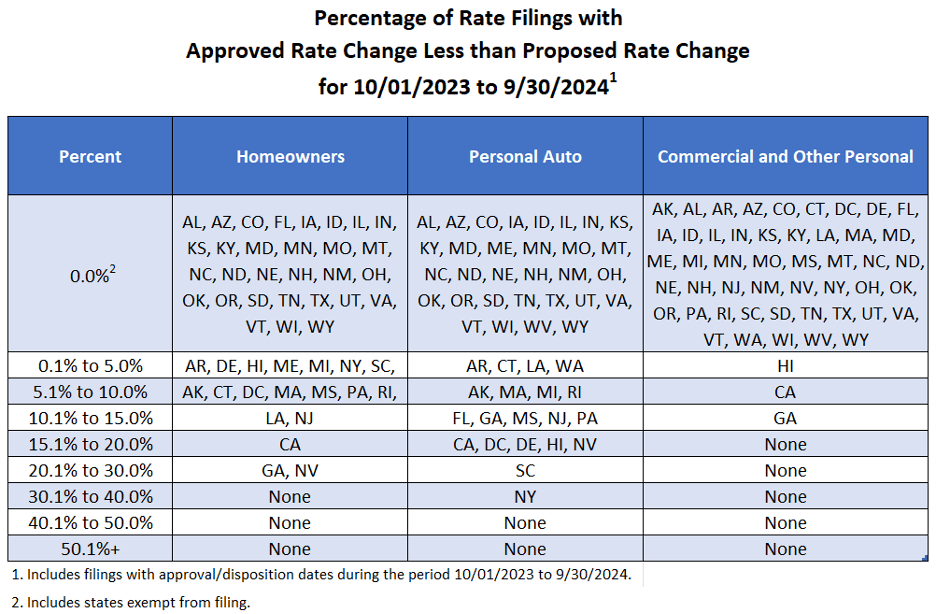
State filings are becoming more complex and time sensitive. Departments of Insurance (DOIs) are scrutinizing filings more closely, often requiring detailed justifications and supplemental information. Meanwhile, insurers are under pressure to accelerate time-to-market for product changes, particularly as competitive cycles tighten.
Regulators, too, are modernizing. The NAIC has continued to evolve the SERFF platform and has pushed for more consistency in electronic submissions. However, integration challenges remain, especially for carriers that manage filings with legacy systems or siloed processes.
In this environment, operational efficiency isn’t just a convenience; it’s a strategic requirement.
Recent trends highlight the shift:
- Rate modernization initiatives in several states have shortened filing windows, demanding quicker response times
- Data calls and reporting obligations have become more frequent and more detailed, increasing documentation overhead
- Regulatory objections have grown in complexity, requiring better documentation and internal collaboration to resolve quickly
A centralized solution like PK1Cloud Filings helps insurers keep pace with these changes by unifying processes and reducing administrative drag.
Eliminating Redundant Systems: A Broader Organizational Benefit
Beyond compliance, the carrier in this case study saw broader organizational benefits. By removing the need for an internal Access database, they eliminated the overhead of maintaining an outdated system that required IT support and periodic troubleshooting.
In many insurance organizations, regulatory teams are forced to rely on systems that are not purpose-built for state filings. PK1Cloud Filings, by contrast, is designed specifically for the insurance industry, with functionality that aligns with how regulatory teams actually work.
This alignment leads to several ongoing advantages:
- Better collaboration between actuarial, product development, and legal teams
- Consistent version control, so everyone sees the same data in real time
- Structured workflows that make onboarding and training new team members more straightforward
Why It Matters
Compliance is too important and too resource-intensive to be slowed by duplicative data entry and outdated tools. This case study proves that it’s possible to achieve:
- Reduced operational costs
- Improved compliance accuracy
- Faster time-to-market
- Greater audit readiness
- Elimination of redundant internal systems
All by centralizing and automating what was formerly a manual, high-friction process.
Take the Next Step
Whether you’re looking to streamline workflows, reduce filing errors, or improve coordination across teams, PK1Cloud Filings offers a modern solution built for the complexity of today’s insurance environment.
Visit our website to learn more or get in touch with us directly to discuss your current state filings process. We’re happy to provide tailored guidance based on your filing needs and internal systems.